When Beth Silverstein tested positive for the BRCA1 gene mutation, she knew she had to make some tough decisions about her health. But she wasn’t alone. Her faith, her family and her multidisciplinary healthcare team at UNC Lineberger were with her every step of the way.

When Beth Silverstein looks into the mirror, it’s easy to see her resemblance to her mother, Leslie Silverstein. The two share the same dark hair and eyes and the same olive skin. At five feet three inches tall, they’re virtually the same height. “I’m her ‘mini-me’,” laughs Beth. “We’ve always been very close.”
However, while the similarities in their outward appearances are obvious, Beth didn’t know—and, as a carefree young woman in her late twenties, didn’t really want to know—if she had inherited her mother’s genetic history that predisposed her to cancer.
“We are of Ashkenazi Jewish descent, an ethnicity with a much higher risk of certain gene mutations that frequently lead to breast and ovarian cancer,” explains Beth. “My grandmother died at age 36 of breast cancer, and my mother was diagnosed with the same disease at age 39. My mom went through genetic testing because so many of our family members had battled various kinds of cancers, and she encouraged me and my sister Amy to be tested as well. But I didn’t want to. I guess you could say I was in denial, like an ostrich with its head in the sand.”
Beth completed her undergraduate studies at UNC-Chapel Hill in 1999 and later pursued her master’s degree at UNC’s Kenan-Flagler Business School, where she had the opportunity to study abroad in New Zealand. But before leaving, she went for her routine mammogram. That visit was a turning point in Beth’s life.
“While I was in New Zealand, I received a voicemail from my doctor, encouraging me to schedule an appointment upon my return to the U.S. because they needed to do additional breast imaging,” Beth says. “Fortunately, those additional mammography and ultrasound results were all good, but I realized that knowledge is power, and I wanted to be proactive with my health. So I pursued genetic testing.”
Beth’s genetic results came back in just a couple weeks. She tested positive for the BRCA1 gene mutation, the same mutation her mother and grandmother had. She was heartbroken.
Next steps and choices
“In April 2008, Beth came to UNC to meet with me and my colleague Catherine Fine, MS, who is a genetic counselor. We reviewed Beth’s genetic results and mapped out her family history, and we determined that her risk for developing breast cancer was in the upper 80th percentile,” explains James P. Evans, MD, PhD, a UNC Lineberger member and the Bryson Distinguished Professor of Genetics and Medicine at UNC-Chapel Hill. “Catherine and I discussed her options with her, which included having a bilateral mastectomy, or she could choose enhanced surveillance consisting of regular visits to our high-risk breast cancer clinic for periodic breast exams, mammograms and MRI’s.”
But that wasn’t the only difficult decision Beth would have to make. Due to her genetic history, Beth had a 50 percent chance of developing ovarian cancer. During their counseling session, Evans explained to Beth that as she aged, her risk would substantially increase. “As a geneticist, I become very nervous when patients like Beth reach their mid-40s and have not taken preventive measures,” says Evans. “Unfortunately, there are no good modalities for detecting early-stage ovarian cancer; the symptoms are vague at best and often mimic other health issues. Once a woman has the disease, it can be extremely difficult to treat.”
Beth was overwhelmed by the news but decided to approach the situation with a positive attitude. During the next five years, she went for regular six-month checkups with surgical oncologist Keith Amos, MD. But on multiple occasions, Beth experienced anxiety after finding benign lumps in her breasts. In 2013, Amos told Beth it was time to take the next step; she needed to consider having her ovaries removed because that would reduce her risk for developing both breast cancer and ovarian cancer. But first, she’d need to explore her fertility preservation options.
Then, just months after their discussion, Amos died of a sudden aortic dissection. Beth was devastated. “Dr. Amos had been my calming force, my encourager during this entire process,” Beth says. “I felt lost without him.”
“It goes without saying that I have had a rock star health care team,” says Beth. “Information is power, and they helped me make informed, thoughtful decisions. I can’t think of a better group to have in my corner. Lineberger is beyond lucky to have this multidisciplinary team.”
Fertility and the future
Beth was 36 at the time, and she knew her biological clock was ticking. So in July 2013, she met with Jennifer Mersereau, MD, and Marc Fritz, MD, at UNC Reproductive Endocrinology & Infertility to discuss harvesting her eggs. Fritz explains that even with the removal of her ovaries, as long as she has a uterus, Beth could still carry a child. “Her preference would be to have a biological child, so her options were to go through egg retrieval and then to have the eggs frozen for later fertilization and implantation,” he says. “If that didn’t work, any future pregnancy would require donor eggs.”
In March 2014, Beth underwent the first of two egg retrieval cycles, which yielded three mature eggs. She decided to go through the procedure again, and three months later, nine more mature eggs were retrieved. Both times, the eggs were frozen through cryopreservation. Beth had done what she could to protect her fertility.
Choosing her new team
After her egg preservation, Beth put her health concerns on the back burner for nearly a year before choosing to work with oncologist Carey Anders, MD. “Dr. Anders is fabulous and made me feel in control yet cared for,” says Beth. “Soon after we met, she introduced me to another surgical oncologist, David Ollila, MD, who recommended that we perform a bilateral mastectomy as soon as I could free up time in my professional schedule. That was tough to hear, but given my family genetic history and my personal genetic risk for cancer, it was the right step to take.”
While the recommendation to have a bilateral mastectomy may seem aggressive to some, Ollila says the opposite is true in BRAC gene mutation carriers. “Surveillance is not the same as prevention. Obtaining annual breast imaging only serves to try to detect the cancer early. It doesn’t prevent the cancer from forming.
If Beth had chosen to forgo surgery and decided instead to take a ‘wait and see’ attitude, it’s very likely that at some point in the near future, we would be discussing a cancer diagnosis, followed by surgery, radiation and chemotherapy. And that’s IF we caught it early enough. Beth didn’t make this decision lightly; it was a thoughtful, rational choice, and a wise one, in my professional opinion, supported by concrete genetic evidence.”
Timeline
On February 3, 2015, Ollila began the first part of Beth’s bilateral mastectomy—taking out the breast tissue—and then plastic surgeon Lynn Damitz, MD, came in behind him to begin the reconstruction process. The second phase of Beth’s surgery would be completed in the summer of that same year.
In June 2015, Beth met with Evans and Fine again, this time to review her lab work and to further discuss the surgical removal of her ovaries. “They were concerned about my age—I’ll turn 40 in 2017—and we talked about how my risk for ovarian cancer was increasing with each passing year,” says Beth. “I felt this cloud of stress hanging over me; I knew it was time to talk with a surgeon.”
In November 2015, Beth had an ultrasound prior to her consult with gynecological oncologist Vicki Bae-Jump, MD, and to her surprise, she had a cyst on one of her ovaries. While test results showed the growth was benign, she decided to move forward with her surgery—sooner, rather than later. “I didn’t want to play with fire,” she says, “And I refused to live with this ongoing worry, wondering if they’d find cancer at my next checkup. After meeting with Dr. Bae-Jump, I scheduled my surgery.”
In February 2016, Beth had a salpingo-oophorectomy, which is the removal of the fallopian tubes (salpingectomy) and ovaries (oophorectomy). The two-and-a-half hour surgery went well, but it immediately sent Beth into menopause. She’s now dealing with the after-effects that include hot flashes, insomnia and “foggy brain.” But for Beth, this is the new normal. While the surgeries have changed her, both physically and emotionally, she feels empowered as she enters the next decade of her life.
“Some people ask me why I decided to take, what they perceive to be, such radical steps. I won’t lie, it was hard,” she says. “But the moral of this story is that you need to know your family history, and recognize that genetics affect every generation. I’m not a victim; I took control of my health, making the choices that were right for me. Now I get to live my life without fear of what’s going to happen. That’s liberating.
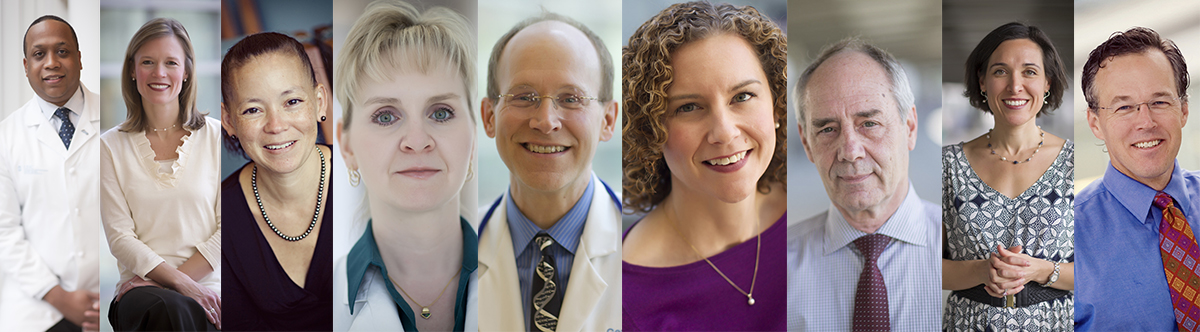
Beth’s care team at UNC, from left to right: Keith Amos, MD (deceased); Carey Anders, MD; Victoria Bae-Jump, MD; Lynn Damitz, MD; James Evans, MD, PhD; Catherine Fine, MS, CGC; Marc Fritz, MD; Jennifer Mersereau, MD; David Ollila, MD
